What’s up ? This is THE stephane ANDRE. With my training, I’m interested in biomechanics to avoid injuries. I read « Sport Medicine Media Guide » and I learned some good stuff.
Methicillin-Resistant Staphylococcus aureus (S. Aureaus), or MRSA, is a bacterium that creates skin infections and other types of infections. The first time that MRSA was seen in US hospitals during the 1970s. Recently, there is a new strain of MRSA know as Community Acquired Methicillin-Resistant Staphylococcus aureus, or CA-MRSA, has left hospitals and began to spread in the community.
This is the strain that is prevalent among athletes. The difference between CA-MRSA and Healthcare-Associated MRSA (HA-MRSA) is in their effects. CA-MRSA usually creates skin infections while HA-MRSA causes bloodstream, urinary tract and surgical site infections. This make CA-MRSA less dangerous than HA-MRSA. Another difference is that CA-MRSA is more vulnerable to antimicrobial.
Symptoms
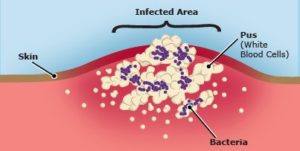
Signs of infections are :
-
Redness
-
Warmth, Swelling
-
Pus
-
Pain at sites where there are skin wounds
-
Abrasions or cuts
MRSA has the ability to spread to other organs in the body and when that happens, symptoms are more severe.
At this stage, symptoms are :
-
Fever
-
Chills
-
Low blood pressure
-
Joint pain
-
Severe headaches
-
Shortness of breath
-
An extensive rash over the body
These more advanced systemic symptoms require immediate medical attention.
Treatment
The 1st choice for treating MRSA skin infection is to use an antibiotic that has been created to kill bacteria with mild side effects. Most early infections with no widespread symptoms can be treated with oral antibiotics. Because of the nature of this decease and antibiotic options, many patients think they’re « cured » after only a few doses and decide by themselves to stop taking the prescribed drugs. However, MRSA is able to re-infect the patient and become resistant to antibiotics used previously.
For moderate to severe infections, treatment may be with intravenous antibiotics.
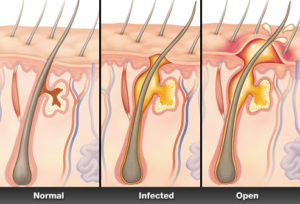
These infections associated with deep abscesses or boils require open surgical drainage in addition to antibiotic therapy. Most infections resolve in 7-10 days with an adequate treatment despite the fact that a deep abscess can take up to 4 weeks to eradicate the infection by resolving the abscess cavity.
Early identification and treatment of MRSA infections decrease the amount of playing time lost and decrease the chance that the infection will become severe. Skin may be protected by protective clothing or gear designed to prevent skin abrasions or cuts.
Prevention
It’s necessary that athletes have good personal hygiene but it must be added that athletes and visitors to athletes facilities must also keep their hands clean by washing them often with soap and water or using an alcohol-based hand rub. The minimum is to have clean hands before and after sports and activities. For example when we use weight training equipment that is shared by all gym members, it’s important to have clean hands after using toilette or when someone is injured taking care the wounds (including changing bandage).
Ordinary and antimicrobial soaps are effective for washing hands. It’s noted that liquid soap is a better option because it’s not possible to share this type of soap compared to bar soap. Alcohol-based hand sanitizer that contain at least 60% alcohol are the perfect choice.
Athletes should shower immediately after exercise and shouldn’t share soap and towels. Washing all uniforms and clothes after each use is important. Athlete should avoid sharing items that are in contact with the skin and avoid sharing personal items as they contact the skin. Fortunately, most surfaces don’t provoke a risk of spreading staph and MRSA.
Athletes who have had MRSA
Several high school, college and professional athletes have contracted MRSA infections. There have already been epidemics among athletes on the same team. A study published in « The New England Journal of Medicine » shows an infection MRSA among St. Louis Rams professional football franchise (USA) athletes. During a single season, MRSA infections were found among 5 of 58 Rams athletes (9 percents) that was tested. All infections developed on areas of the body that are common places for turf injury.
Stats
-
Today, MRSA accounts for about 50-70% of the S. Aureus infections that are present in healthcare facilities across the world.
-
Statistics fro the Kaiser foundation in 2007 indicated that approximately 1.2 million hospitalized patients contract MRSA infections.
-
Serious MRSA infection is still predominantly related to exposure in the healthcare setting, where approximately 85 percent of all serious MRSA infections occur.
-
Fortunately, in children under 18 years old, mortality rates are much lower (1%), even though the number of hospitalized children with MRSA has almost tripled since 2002.
Subscribe to my newsletter and share this article if you think it can help someone you know. Thank you.
-Steph
P.S. If you’re in Miami and you like Caribbean food, go to my cousin’s bistro to eat Haitian food, click here .
Hi Stephane,
I have a question for you, if you don’t mind.
Background: I believe I have an impetigo bacterial infection. It says that it is caused by either a MRSA or strep bacteria. I’m 48 and have never had strep as far as I know. I’m getting an all-natural antibiotic that I can take internally, and I have the option of applying it externally to the skin wounds if that would be beneficial. (Underlying I have had fungal candida and Lymes, and I’m on an excellent protocol for cleansing the body from those. I’ve been looking for ore than 20 years, and finally found one that works amazingly well and is high quality. Non-GMO, organic, no fillers or excipients. ! I’ve been eliminating lots of parasites on a daily basis. I had no idea I even had them! They are the carriers of the candida, lymes, mold, bacterial infections, etc.
My question is about your drawing or pictures of the MRSA infections. I’ve been using a drawing salve to try to figure out what is going on, and it draws out white pustules that soften over several day’s times, then drain, and a honey-colored crusty something forms around or on top of the pustules. I read about Impetigo, and that’s exactly how the two symptoms they describe. So when I found it could be tracked back to a MRSA infection, I was interested to know this: the picture (at tope of page) shows the white blood cells that form the pus, and the blue dots are the bacteria. So when I just leave them alone and let them process, when they drain, the bacteria comes out with the pus? Would that be correct? There have been a few times where the pustule has been so taught that it was painful, so I’d push gently and the faucet would start. Does my doing that have a negative effect on getting bacteria out of the body?
I realize that this is not a cure for MRSA/Impetigo, but I’d like to do my best at managing the process until the antibiotic arrives. It’s a combination of 3 essential oils (Do Terra: On Guard, Tea Tree Oil and Oregano). It works as a broad-spectrum antibiotic without having the negative effects of killing off healthy cells or healthy flora.
Is it possible that I could have both Impetigo and MRSA (and even other bacterias) all at the same time, and they whatever bacteria is present would drain out of the pustules? I think the impetigo is fairly new. I figured out I had it when my hair starting tangling and matting quite badly. Only one bacteria tied to that and it’s impetigo. And then when I saw how impetigo presents on the skin, it was easy to figure out. I would say it’s systemic in that I have had active wounds (healing or forming) on all 4 extremities. Arms and legs. Nothing on torso or face.
I have seen white squigglies under my skin, and when I put the drawing salve on them, that’s where the pustules come out, And one weekend I got a rash covering the entire knee to shin on both legs, and it itched horribly. I went to all my natural cures, and none of them worked to relieve the itching, so I used the drawing salve and all kinds of pustules and some other little black specs came out over the process of a month and several salves. It did relieve the itching after the first day or two.
Once the antibiotic (all natural) arrives, would it help the process of killing it off go faster if I continue using the drawing salve? Or would it be best to just take the antibiotic and heal from the inside. Since it’s so wide-spread, I wasn’t sure how long it would take the antibiotic to do its job. I do know I’ll know when it’s done since I have had a lot of symptoms I can see and feel.
I have plenty of pictures as I track when I salve. I don’t know if any of them would tell you more than they do me. If you are able to reply, I do have one more question related to Lyme coinfections. But I’ve written more than enough for now. Thank you!
Hello,
Wow, big case.
First:
Yes, you can have MRSA and impetigo at the same time because impetigo is contagious and can be transmitted from person to person. It’s usually caused by one of two bacteria: Staphylococcus aureus or Streptococcus pyogenes (also called group A streptococcus, which also causes strep throat). MRSA is also becoming an important cause of impetigo.
Treatment
Impetigo is usually treated with antibiotics, which can be taked by mouth. In very mild cases, a topical antibiotic can be used. The best way to treat MRSA is to properly treat wounds (incision and drainage by a health care provider), to cover with a clean, dry bandage and, in some cases, antibiotics (to which the body is susceptible).
In your case, you’ll use a natural antibiotic and I don’t know the results, but for a conventional antibiotic of a pharmaceutical company, you must use it for 7 to 10 days. I’m waiting a little longer for your natural antibiotic to see results.
I advise you to contact a doctor because you said it has spread. It would be safer to have a doctor in this process in case of complications. And the doctor will be able to see if the natural antibiotic is working or not.
I hope I helped you.
-Steph